CAMBRIDGE, MASS.- In a uniquely deep and detailed look at how the commonly used anesthetic propofol causes unconsciousness, a collaboration of labs at the Picower Institute for Learning and Memory at
MIT shows that as the drug takes hold in the brain, a wide swath of regions become coordinated by very slow rhythms that maintain a commensurately languid pace of neural activity. Electrically stimulating a deeper region, the thalamus, restores synchrony of the brain’s normal higher frequency rhythms and activity levels, waking the brain back up and restoring arousal.
“There’s a folk psychology or tacit assumption that what anesthesia does is simply ‘turn off’ the brain,” says Earl Miller, Picower Professor of Neuroscience and co-senior author of the study in eLife. “What we show is that propofol dramatically changes and controls the dynamics of the brain’s rhythms.”
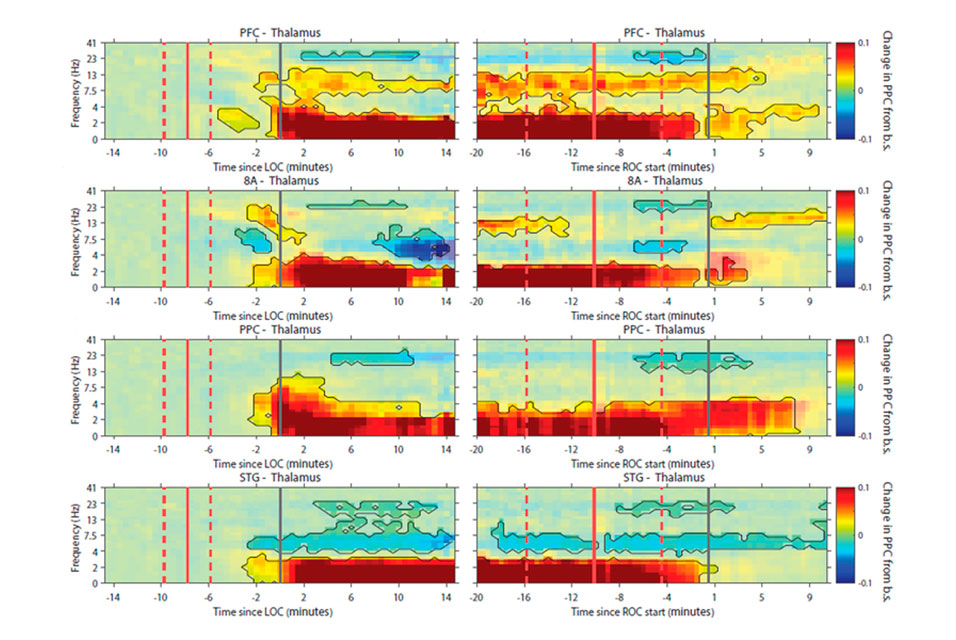
Conscious functions, such as perception and cognition, depend on coordinated brain communication, in particular between the thalamus and the brain’s surface regions, or cortex, in a variety of frequency bands ranging from 4 to 100 hertz. Propofol, the study shows, seems to bring coordination among the thalamus and cortical regions down to frequencies around just 1 hertz.
Miller’s lab, led by postdoc Andre Bastos and former graduate student Jacob Donoghue, collaborated with that of co-senior author Emery N. Brown, who is the Edward Hood Taplin Professor of Medical Engineering and Computational Neuroscience and an anesthesiologist at Massachusetts General Hospital. The collaboration therefore unified the Miller lab’s expertise on how neural rhythms coordinate the cortex to produce conscious brain function with the Brown lab’s expertise in the neuroscience of anesthesia and statistical analysis of neural signals.
Brown says studies that show how anesthetics change brain rhythms can directly improve patient safety because these rhythms are readily visible on the EEG in the operating room. The study’s main finding of a signature of very slow rhythms across the cortex offers a model for directly measuring when subjects have entered unconsciousness after propofol administration, how deeply they are being maintained in that state, and how quickly they may wake up once propofol dosing ends.
“Anesthesiologists can use this as a way to better take care of patients,” Brown says.
Brown has long studied how brain rhythms are affected in humans under general anesthesia by making and analyzing measurements of rhythms using scalp EEG electrodes and, to a limited extent, cortical electrodes in epilepsy patients. Because the new study was conducted in animal models of those dynamics, the team was able to implant electrodes that could directly measure the activity or “spiking” of many individual neurons and rhythms in the cortex and thalamus. Brown said the results therefore significantly deepen and extend his findings in people.
For instance, the same neurons that they measured chattering away with spikes of voltage 7-10 times a second during wakefulness routinely fired only once a second or less during propofol-induced unconsciousness, a notable slowing called a “down state.” In all, the scientists made detailed simultaneous measurements of rhythms and spikes in five regions: two in the front of the cortex, two toward the back, and the thalamus.
“What’s so compelling is we are getting data down to the level of spikes,” Brown says. “The slow oscillations modulate the spiking activity across large parts of the cortex.”
As much as the study explains how propofol generates unconsciousness, it also helps to explain the unified experience of consciousness, Miller says.
“All the cortex has to be on the same page to produce consciousness,” Miller says. “One theory about how this works is through thalamo-cortical loops that allow the cortex to synchronize. Propofol may be breaking the normal operation of those loops by hyper synchronizing them in prolonged down states. It disrupts the ability of the cortex to communicate.”
For instance, by making measurements in distinct layers of the cortex, the team found that higher-frequency “gamma” rhythms, which are normally associated with new sensory information like sights and sounds, were especially reduced in superficial layers. Lower-frequency “alpha” and “beta” waves, which Miller has shown tend to regulate the processing of the information carried by gamma rhythms, were especially reduced in deeper layers.
In addition to the prevailing synchrony at very slow frequencies, the team noted other signatures of unconsciousness in the data. As Brown and others have observed in humans before, alpha and beta rhythm power was notably higher in posterior regions of the cortex during wakefulness, but after loss of consciousness power at those rhythms flipped to being much higher in anterior regions.
The team further showed that stimulating the thalamus with a high-frequency pulse of current (180 hertz) undid propofol’s effects.
“Stimulation produced an awake-like cortical state by increasing spiking rates and decreasing slow-frequency power,” the authors wrote in the study. “In all areas, there was a significant increase in spiking during the stimulation interval compared to pre-stimulation baseline.”
In addition to Miller, Brown, Bastos and Donoghue, the paper’s other authors are Scott Brincat, Meredith Mahnke, Jorge Yanar, Josefina Correa, Ayan Waite, Mikael Lundqvist, and Jefferson Roy.
The National Institutes of Health and the JPB Foundation provided funding for the study.
Reprinted with permission of
MIT News